As an introduction to the readers, I practiced hematology and medical oncology for 30 years at the University of Washington and Oregon Health & Science University. I am currently enrolled in the master’s program in Applied Artificial Intelligence at University of San Diego.
What comes to mind when you try to envision healthcare of the future? Perhaps you imagine characters from Star Trek or in other science fiction portrayals, where a human or humanoid doctor interacts with a patient much like doctors of today, a scanner is run over the body, and out pops the diagnosis. This is how a Hollywood scriptwriter might conceive of medical care in the future, but what might a physician think, especially in the rapidly advancing era of computing technology and of course, artificial intelligence?
Since ancient times, the basic workflow for the physician has been to collect information from the patient, obtain relevant diagnostic testing, all the while formulating diagnostic hypotheses in ranked estimated likelihood, perform secondary testing for confirmation and stratification, then initiate therapy (if available), and finally, assess the response to treatment, revising the hypotheses, if indicated. While the information intake process is sometimes abbreviated based on the situation, the basic elements of the workflow have remained unchanged over the centuries.
In the clinic of the future, humans will likely remain a critical element of the clinical encounter, however, technology has and will continue to replace some of the more routine parts of the clinic visit. For example, the acquisition of vital signs, already automated in many clinics, may soon be obtained by IoT-connected sensors, with data automatically entered into a patient’s chart. By now, it is safe to say that most people have seen their doctors interact with laptop or notebook computers in the exam room, entering data, scanning snippets of information, and reading chart notes. In the past couple of years, clinicians have also made use of audiovisual equipment, and telemedicine encounters are now accepted as mainstream. Less apparent but increasingly prevalent is the increasing number of diagnostic imaging platforms and cardiac devices that have incorporated AI or machine learning software.
From the physician’s standpoint, however, I feel that the most significant changes in how medicine will evolve are not necessarily the hardware components you can see (such as the new sensors, the mobile apps, the handheld and implanted devices) but what happens behind the scenes.
The foundation for much of the change in healthcare has been the implementation of the electronic health record (EHR). Whereas in the past, patient information resided in paper charts, data now reside in digital format, accessible for analysis as well as auditing, which has been a boon to hospital systems. But while financial information (purchase price, usage data, expenses and billing data) is entered by clerical staff into electronic forms, much of the information stored in the EHR is unstructured data. This includes free text information (such as provider notes), diagnostic imaging, scanned documents, and audio/video data. Physicians have resisted entering clinical information into pre-determined forms or clicking on checkboxes, as these may not contain all the relevant nuances about a case. Instead, they prefer to dictate or type their notes, often using jargon, as well as grammatically improper and imprecise language. While understandable to other humans, this text-based information is not readily accessible for computer-based analysis. Until recently, there was no feasible way to parse a physician’s abstruse textual record to extract machine-readable information that could be used for clinical research or to ensure proper documentation. However, the advent of Natural Language Processing (NLP) holds the promise of being able to properly interpret and process this textual information into a format suitable for data analysis.
NLP will impact a physician’s workflow in other important ways. For one, more accurate voice-to-text recognition will lead to better transcription accuracy, and the ability to quickly generate precise and complete notes will be heartily welcomed by physicians. However, being able to extract key information from a progress note, as well as hospital admission and discharge summaries, will be a boon not only to the billing team but also to clinical research teams. Identification of salient eligibility factors by scanning physicians’ notes, has the potential to increase accrual to clinical trials.
Let’s get back to the physician, who must formulate a differential diagnosis of probable conditions and select the best available therapy. In the 1950s, a learned physician felt comfortable with his/her knowledge base and could expect that it would take about 50 years for medical knowledge to double in amount. At that time, keeping up with new developments would not require much effort. But by 2020, the knowledge doubling time was reduced to 73 days. Despite this, the post-graduate education maintenance pathway has not changed significantly. Physicians are still expected to keep up with efforts such as journal reading, perhaps attending key conferences and seminars, and maintaining board certification, but the efforts to support physicians in this endeavor are highly variable and spotty. Textbooks have evolved from physical tomes to digital publications, as it was impossible for books to keep up with the latest critical information. Journal articles are almost always accessed online now, and the number of relevant journals available to peruse, has also increased. And besides staying abreast of the medical literature, it is also advisable to keep up with advances in the pharmaceutical industry, as many developments are made public through those channels.
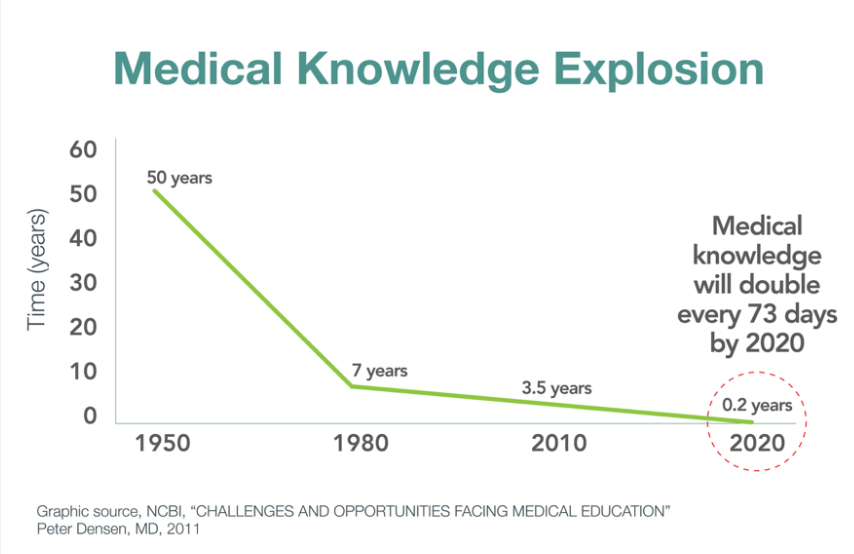
Fig 1. How long will it take before medical knowledge is doubled? Source.
Most, if not all, physicians have a repository of curated journal articles that they find relevant to their practice. Having them for ready access might save time from having to use MEDLINE search to locate the desired reference on demand. Some use reference managers to store and organize articles, but as the collection grows, finding an article can be almost like searching from scratch again. Rather than forcing physicians to use archaic search engine technology, an NLP interface might be more accurate and helpful. It might be possible to make more direct clinical queries (such as “what is the best empiric antibiotic for community acquired pneumonia?”) and the response will not only be the desired drug, but a culled set of references that support that recommendation. At present, this wonderful query interface is yet unavailable.
Another common approach to getting access to the current standard of practice is to consult with an expert. I would have a network of trusted experts that I could call on to discuss cases and to learn about the latest developments, not all of which were available online. I have found that, at times, new “clinical breakthroughs” need to be reviewed by experts in the field, to determine if these new findings are truly practice-changing, or if there are details in the study protocol that warrant caution and require additional data. In many academic centers, there are sub-specialists who focus on just a specific subset of a disease, networking with other narrowly-focused researchers, so as to keep up with advances. These individuals are exemplars of the expert system approach, but while valuable in their role, they are not always accessible. However, with the availability of practice data, this may change, as “it’s much better to see what a doctor does, rather than ask them what they’re doing.” Analysis of outcomes data from a large healthcare system has already been shown to outperform national association guidelines in the management of diabetes mellitus. It may therefore someday be possible for a physician to obtain clinical guidance on accepted therapy by examining the practice patterns of those who have treated similar patients, and decide what treatment options to consider.
It is now possible to capture and process quality data than ever before. New machine learning, image, video and natural language processing tools will provide physicians with more meaningful analytics stemming from this data. Computer hardware has improved, with higher performing chips and architectures. Providers of cloud computing platforms are competing to offer AI/ML-based analytics and data processing. All of these promise to enable the physician to make better decisions, using data-driven recommendations that would not have been available in the past. Physicians empowered with these tools will have a clear advantage over those who do not. It will be especially challenging for the non-networked practitioner to provide the state-of-the-art care that patients will come to expect.